Abstract
The association of iron toxicity with vital organ dysfunction has been extensively investigated in transfusion-dependent-thalassemia (TDT). However, pituitary iron load and its effect on function have been infrequently addressed. Growth delay, hypogonadism and infertility resulting from iron-induced pituitary toxicity are still prevalent, impacting clinical care and patients' quality of life. Early recognition and timely intervention can potentially prevent irreversible damage and restore partial function.
Aims
We aimed to determine pituitary iron load and anterior pituitary volume by MRI in various age groups of TDT and examine their association with systemic and organ-specific iron measures. Additionally, we attempted to stratify the occurrence of abnormal anterior pituitary function by these MRI findings. Identifying such risk thresholds could assist in establishing timing and effectiveness of treatment intervention.
MRI (1.5T) measurements of anterior pituitary iron (R2) and volume (Vol) were compared to normal controls (Noetzli 2011) with resultant Z-scores. Mean annual ferritin was calculated and cardiac and liver iron concentration (LIC) were determined by MRI-T2* and superconducting quantum interference device (SQUID) biosusceptometry, respectively. Pituitary hormones (LH and FSH) and growth hormone (Z scores for IGF-1 and IGF-BP3) were determined.
Results
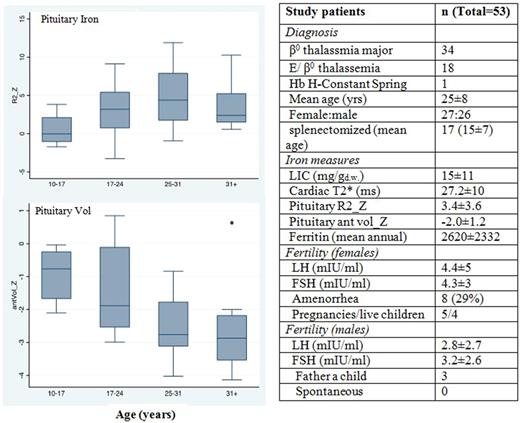
Fifty-three TDT patients (51% females) age 25±8 years, (range 10-45 years) were enrolled. Thirty-three (62%) had a ZR2 value >2 (mean 5.4) indicating iron accumulation above 97.5th percentile. Thirty-two patients (60%) had a Z-score for anterior-volume (ZVOL) of less than -2 (mean -2.8) indicating gland shrinkage below the 2.5th percent. In 23 patients (43%) both ZR2 and ZVOL exceeded these thresholds. ZR2 inversely correlated with ZVOL; r =-0.32, p<0.02. Pituitary iron increased with age and differed between patients <18 yr (n=14) and those 18-45 yr (n=39) with a mean ZR2 at 0.9±0.6 and 4.3±0.5, respectively (p<0.001). Anterior pituitary volume declined in older patients, lagging after the iron accumulation (Figure).
LH/FSH values and ZR2 showed inverse correlation: r = -0.27 (p<0.03) and -0.3 (p< 0.006) respectively. ZVOL and LH/FSH demonstrated a positive correlation: r = 0.40, p<0.05 and 0.37, p<0.003, respectively. Z(IGF-BP3) but not Z(IGF-1) had an inverse correlation with ZR2: r = -0.5 (p<0.001).
ZR2 > 4 was found to be a significant predictor for gland shrinkage; Zvol < -2 was present in 17/33 patients with a ZR2>4 compared to 3/20 with a ZR2<4 (p<0.009). Receiver operator (ROC) analysis confirmed it with an AUC of 0.68. ZR2 >4 was also predictive of presence of clinically important cardiac (T2* <20ms, AUC=0.92, p<0.001) and hepatic iron (LIC >10mg/gd.w., AUC= 0.74, p<0.005). Mean ferritin significantly correlated with ZR2 (p<0.001) but not with the gland's volume.
Conclusions
Anterior pituitary iron assessed by MRI, increases with age and correlates with total body iron burden in TDT, suggesting cumulative iron toxicity. It results in a decrease in gland size and impaired gonadotropin and growth hormone secretion. Pituitary iron exceeding ZR2 >4, appears to be a significant predictor for change in gland size, that also is associated with cardiac and liver iron-overload. Pituitary MRI and the concomitant liver and cardiac iron quantification can identify patients at high-risk for further pituitary damage, suggesting that early intervention can potentially prevent additional decline in hormonal secretion.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal